Drug – Nutrient Interactions
How Drugs and Nutrients Interact
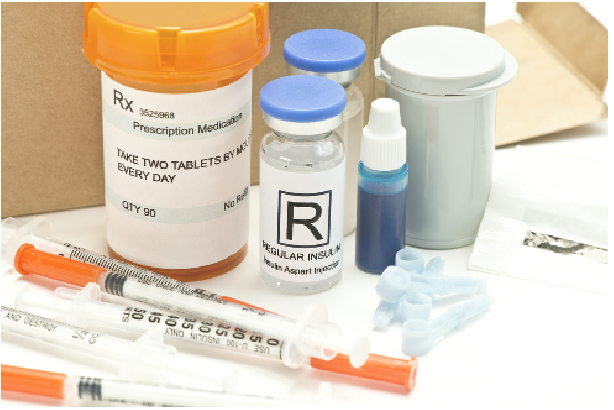
Both prescription and over-the-counter medications can affect the way your body uses nutrients in food. In addition, certain foods or nutrients in food can affect the action of medications.
A drug-nutrient interaction is the effect of a medication on food or a nutrient in
food. Medications interact with foods and nutrients in several ways. Medications can
decrease appetite or change the way a nutrient is absorbed, metabolized, or excreted.
A food-drug interaction is the effect of food or a nutrient in food on a medication.
Dietary nutrients can affect medications by altering their absorption or metabolism.
The food you eat could make the medications you take work faster, slower, or even
prevent them from working at all.
Such interactions raise concerns that medications may lead to nutritional deficiencies or that your diet may change how a medication works. This does not mean that if you are taking a medication you need to use a vitamin and or mineral supplement. There is little chance that taking a medication for a short time, such as a ten-day treatment, will affect your nutritional status. However, use of some medications for months or years may affect your nutritional health.
Children, older adults, pregnant women, people who are poorly nourished, and people with a chronic disease are at greater risk of medications affecting their nutritional health. Changing the diet to include more foods rich in vitamins and minerals is preferred to taking vitamin or mineral supplements. In fact, vitamin and/or mineral supplements taken in excess can affect how a medication works.
Drug-Nutrient Interactions
Medications, both prescription and over-the-counter, can affect how the body uses nutrients. For individuals taking medications for long periods of time drug-nutrient interactions may lead to vitamin or mineral deficiencies.
- Medications can decrease appetite or cause nause
 a, vomiting, an unpleasant taste, or dry mouth. This can affect nutritional health
by causing poor food intake.
a, vomiting, an unpleasant taste, or dry mouth. This can affect nutritional health
by causing poor food intake.
Example: Appetite suppressants are medications that directly affect food intake by depressing appetite.
Example: Several cancer medications and treatments may cause nausea, vomiting, sore, or dry mouth resulting in poor food intake. - Medications can decrease nutrient absorption.
Example: Laxatives can decrease the absorption of many vitamins and minerals. Laxatives cause food to move rapidly through the body causing poor nutrient absorption.
Example: Some anticonvulsants can decrease folate absorption. - Medications can slow down nutrient production.
Example: Vitamin K is produced by bacteria in the intestines. Antibiotics kill harmful bacteria, but they can also kill helpful bacteria, including bacteria that produce vitamin K in the intestine. - Medications can interfere with the body’s ability to metabolize nutrients.
Example: Some anticonvulsants alter the activity of liver enzymes, causing increase metabolism of folate, vitamin D and vitamin K. - Medications can increase the loss of a nutrient.
Example: Diuretics remove excess fluid from the body. Some diuretics may also increase loss of potassium along with fluids. Potassium is very important in proper functioning of the heart and other muscles.
Food-Drug Interactions
Food and nutrients can also alter a medication’s effectiveness in many ways.
- Food can increase or decrease the absorption of a drug. Absorbing less than the intended
dose may decrease the effect of the drug. Absorbing more than the intended dose increases
the chance for an overdose effect.
Example: Dietary calcium can bind to the antibiotic tetracycline. As a result the body does not absorb the amount of antibiotic intended.
Example: Drugs are absorbed more quickly into the body when the stomach is empty. Having food in the stomach will slow down a medication’s absorption. Sometimes a medication should be taken with food. Other medications should be taken on an empty stomach, one hour before or two hours after eating. It is important to read the directions to see if a medication should be taken with or without food. - Foods or nutrients may interfere with a drug’s metabolism or a drug’s action in the
body.
Example: Aged and fermented foods contain a chemical called tyramine that interacts with a medication, monoamine oxidase inhibitor. This interaction can result in dangerously high blood pressure.
Example: Vitamin K can decrease the effectiveness of certain anticoagulant medications. - Foods or nutrients may be needed for the removal of a medication from the body.
Example: Liver enzymes prepare medications for removal from the body. These enzymes require nutrients to work properly. If required nutrients are not present, medications may stay active in the body longer than they are supposed to.
Alcohol
Alcohol and medications do not mix well. Alcohol can adversely affect medications as well as nutrients. Alcohol can slow down the body’s metabolism. As a result medications can stay active in the body longer than they were supposed to. In some cases, mixing alcohol and medications can be fatal. A rule of thumb is to avoid alcoholic beverages when taking prescription or over-the-counter medications.
Nutrient Supplements
Nutrient supplements themselves can result in drug-nutrient interactions. In excessive amounts, vitamins and minerals act like drugs instead of nutrients. Nutrients in excessive amounts may interact with other nutrients or may even be toxic.
Large amounts of zinc can interfere with copper and iron absorption. Similarly, large amounts of iron can interfere with zinc absorption.
The Importance of Following Directions
It is important to follow the directions on how to take a medication. Many people do not take prescription or over-the-counter medications properly. Following the directions on how to take a medication can affect how or if a medication works.
How to Lower the Risk of Drug-Nutrient Interactions
- Eat a healthy diet following the recommended servings from the USDA MyPlate Plan.
- Follow directions on how to take medication (prescription and over-the-counter).
- Read warning labels on both prescription and over-the-counter medications.
- Do not share medications with others or take other peoples’ medications.
- Do not take over-the-counter medications frequently on your own.
- Tell your physician about everything you are taking, including over-the-counter medications, alcohol, and herbal products.
- Tell your physician and pharmacist about any new or intensified symptoms that develop when taking a medication.
- Keep a list of all medications (prescription and over-the-counter) that you use.
- If you have questions, ask your pharmacist, physician, or dietitian for answers.
Questions to Ask Your Physician When You Get a Prescription
- What is the medication for? (medication name, medication purpose).
- How should I take the medication? (how often, how long, storage recommendations, recommendations on consuming food and/or beverages with the medication).
- What should I expect? (expected outcomes, precautions, side effects).
References
Whitney, E.N. & Rolfes, S.R. (2015). Understanding Nutrition, 14th ed., Wadsworth, Cengage Learning, Belmont, CA.
Bernstein, M., & Munoz, N. (2016). Nutrition for the Older Adult, 2nd ed., Jones and Bartlett Publishers, Sudbury, MA.
United States Department of Agriculture. ChooseMyPlate.gov. Accessed at www.choosemyplate.gov
Janice Hermann, PhD, RD/LD
Nutrition Specialist
