Common Ticks of Oklahoma and Tick-Borne Diseases
Ticks transmit a greater diversity of disease-causing organisms to wildlife, domesticated animals and humans than any other vector arthropod. Ticks are also known to cause paralysis, toxicosis and allergic reactions. Tick bites can cause dermatitis (an itching, swelling, inflamed condition of the skin) on the host. In animals, the loss of blood can cause secondary anemia and sometimes death.
Ticks have four “developmental” or life cycle stages known as the egg, larva, nymph and adult (Figure 1). Larvae are sometimes called seed ticks and are slightly smaller than a pin head. Nymphs are larger than a pin head. Adults and nymphs have eight legs, while larvae have six legs.
Ticks are more closely related to spiders than insects. Ticks can be distinguished from insects because their bodies are not divided into distinct segments. A distinct head is lacking, however, mouthparts of varying lengths (depending on the species) protrude from the tick body and are often incorrectly called the head of the tick. There are two main categories of ticks: the Argasidae (soft ticks) and Ixodidae (hard ticks). Soft ticks blood-feed quickly (within an hour). Hard ticks blood-feed for several days to weeks for the adult ticks. Ticks have a very hard outer layer that encloses all of the tick’s organs and allows the tick to withstand environmental stresses. Most of the tick’s life is spent in the off-host environment seeking a host. Some tick life stages are able to survive for a few years without finding a host and taking a blood meal.
The names “dog tick,” “deer tick" and “wood tick” are commonly used to describe many ticks because of their association with dogs, deer and the forest environment. These names are usually used in reference to the engorged (filled with blood) adult females that look much different in appearance than unfed females, the males and all other life stages. These females are much larger, and therefore more visible than the other life stages seen on hosts. These engorged females are often bluish-gray and can be the size of a large olive. Adding to the confusion of the names is the fact that the common names of the tick species have “dog” and “wood” in their names, such as American dog tick, brown dog tick and Rocky Mountain wood tick.
The life cycle and seasonal activity for each tick species vary considerably and will be discussed separately for each.
Figure 1. General life cycle of ticks. www.cdc.gov
Depending on the species, ticks are classified as one-, two- and three-host ticks. As a one-host tick, the larva will attach itself to and remain on a single animal throughout its feeding stages (larva, nymph and adult). Each stage takes a blood meal, with the exception of eggs. After the female completes feeding, she will drop from the host and lay eggs on the ground in masses ranging from several hundred to thousands, then dies. The eggs hatch and the larvae crawl onto the vegetation and transfer to a suitable host as it passes. A two-host tick will utilize one host for both larval and nymphal feeding. A three-host tick will drop from the host between each blood feeding life stage and usually finds a successively larger host with each molt. The majority of tick species are three-host ticks.
The Argasid ticks are represented by two important species in Oklahoma, causing concern for livestock and poultry producers. The Ixodid ticks are represented by a number of species, but only six of the more important species will be considered here.
Soft Ticks
(Argasidae)
Fowl Tick
[Argas persicus (Oken)]
The fowl tick, also known as the “blue bug,” can be an important poultry parasite.The larval,nymphal and adultstages all feed on the same type of host. The adults feed primarily at night and leave the host to hide in cracks and crevices or under debris during the day. Large populations of this tick are capable of killing birds or chickens by removing large amounts of blood during feeding.
The female lays her eggs in cracks and crevices, and after they hatch, the young larvae feed on chickens. The larva may remain on the host four to five days before completing its feeding. After it leaves the host, it molts into the nymphal stage. The nymphs feed mostly during the night, and they feed repeatedly and molt several times before reaching the adult stage. Under favorable conditions, the adult stage can be reached in 45 days. This pest is capable of living long periods of time (years) without feeding.
Spinose Ear Tick
[Otobius megnini (Duges)]
The spinose ear tick (Figure 2) is a common pest of cattle, horses and other domestic and wild hosts throughout Oklahoma. Humans have also been fed on by these ticks. The tick is found in the ear canals of its host. The presence of large numbers can cause severe irritation, inflammation and deafness of the animal. Secondary bacterial infections may cause sloughing of tissue into the ear canal. Infested cattle develop a “flop-eared” condition, which causes discomfort in movement of the head.
The larval and nymphal stages are blood feeders, with the adult being non-parasitic.
Larvae and nymphs are the only life stages found in the ears. The nymph is easily
recognized by spines on the integument and the peanut shape of the body. After the
last feeding, the nymph leaves the host and molts to the adult stage. Males and females
mate on the ground and females lay their eggs under feed bunks, boards and other suitable
protected areas. The newly hatched larvae crawl up
feed bunks or other objects and await contact with a passing host.
Figure 2. Spinose Ear Tick (Otobius megnini) nymph. Credit: D. Kattes Tarleton State University
Hard Ticks
(Ixodidae)
Black-legged Tick
[Ixodes scapularis (Say)]
The black-legged tick (Figure 3), often called the “deer tick," does not have colorful markings and is a three-host tick. It is an important pest of livestock and wildlife in Oklahoma. This tick is a vector of the intracellular bacteria that causes human granulocytic anaplasmosis (Anaplasma phagocytophilum). In addition, this tick transmits several protozoan pathogens to humans, rodents and deer (Babesia microti,Babesia odocoilei), and the Lyme disease spirochete (Borrelia burgdorferi) to humans, dogs, cattle and rodents.
The adults become active in late September and October and are present until March or April. During the early fall, it is often the most common tick on deer and cattle in Oklahoma. The larvae and nymphs are active in the spring and summer and feed on snakes and lizards. In Oklahoma, the black-legged tick is not known to transmit Lyme disease, because the larval ticks do not feed on mice that serve as reservoir hosts for the bacteria.
Figure 3. Deer tick or Black-legged tick (Ixodes scapularis) female (L) male (R). Credit: R. Grantham, Oklahoma State University
Winter Tick
[Dermacentor albipictus (Packard)]
The winter tick (Figure 4) is an important pest of horses, cattle, deer and elk in Oklahoma. Coloration of the dorsal shield varies from none to almost complete covering with white. This tick is the only one-host hard tick in Oklahoma, and therefore spends its entire life cycle on one host, usually deer or cattle. Heavily infested range animals may die from blood loss if left untreated. The winter tick is a vector of anaplasmosis in cattle.
The larval stage becomes active in early October, and the nymphs and adults are most active during the late fall, winter and early spring. Females lay eggs on the ground after feeding, then die. The eggs may hatch in three to six weeks if temperatures remain above 50°F. The larvae cluster together and remain inactive until the onset of cool weather the following fall. This tick is very large when engorged and therefore easily seen on animals.
Figure 4. Winter Tick (Dermacentor albipictus) male (L) female (R). Credit: Mat Pound, USDA Agricultural Research Service, bugwood.org
American Dog Tick
[Dermacentor variabilis (Say)]
The American dog tick (Figure 5) is a common pest of dogs and other small, wild or domestic animals, which are the preferred hosts for the adults of this species. This is a colorful species, having spots of light colors (white, gray, silver) scattered and superimposed over the basic brown and black body color. The American dog tick is a three-host tick. The adults sometimes infest large animals including horses and cattle, but are seldom serious pests of these animals. The adults often feed on humans, and they are a serious pest in high-use wooded recreational areas. The larvae and nymphs feed on small rodents (e.g. mice, rats and rabbits).
The American dog tick is the only known vector of Rocky Mountain spotted fever (RMSF, Rickettsia rickettsii) in Oklahoma. This tick is also a vector of bovine anaplasmosis (Anaplasma marginale), feline cytauxzoonosis (cats, Cytauxzoon felis), canine monocytic ehrlichiosis (Ehrlichia canis) and human monocytic ehrlichiosis (HME, Ehrlichia chaffeensis), and is also known to cause tick paralysis in people and dogs. The larval and nymphal stages have been known to survive two years or longer without feeding. Under suitable conditions, the life cycle from egg to adult may require only three months, but usually the life cycle requires at least one year.
Figure 5. American Dog Tick (Dermacentor variabilis) female (L) male (R). Credit: R. Grantham, Oklahoma State University
Brown Dog Tick
[Rhipicephalus sanguineus (Latreille)]
The brown dog tick (Figure 6) is probably the most widely distributed tick species in the world and is very common in Oklahoma. Dogs are the primary host, but when dogs and their bedding places are in close association with humans, bites to people become more frequent. While this is a three-host tick, all stages often feed on dogs.
The adult ticks are most often found in the ears and between the toes of dogs. The larvae and nymphs are found in the long hair on the back of the neck. The eggs are deposited in cracks and crevices of the dog kennel. These ticks have a tendency to crawl upward and are commonly found in cracks in the roof of dog kennels or ceilings of porches. These ticks will also become established in houses and other buildings that are inhabited by dogs. The brown dog tick transmits a wide range of pathogens to dogs that include Anaplasma platys, Babesia canis, Babesia gibsoni, Ehrlichia canis, Hepatozoon canis and Rickettsia rickettsii.
Figure 6. Brown Dog Tick (Rhipicephalus sanguineus) female (L) male (R). Credit: R. Grantham, Oklahoma State University
Lone Star Tick
[Amblyomma americanum (L.)]
The lone star tick (Figure 7) is a three-host tick and is an important pest of all livestock and wildlife. Larvae, nymphs and adult stages of this species readily feed on humans. The lone star tick is the one most commonly encountered by people during recreational activities in Oklahoma. Ticks quest for hosts along trails and pathways. The larval ticks quest together in a mass and can infest more than 40 different species of wild and domestic birds.
The tick receives its name for the large white spot on the dorsal shield of the female.The male has white markings around its posterior margin. This species has longer mouthparts than the tick species previously discussed.
The lone star tick is active from early spring to late fall. The female is capable of laying 9,000 to 12,000 eggs. This species is one of the most important ticks from a public health standpoint because it is known to transmit human monocytic ehrlichiosis (Ehrlichia chaffeensis), southern tick-associated rash illness (STARI), canine granulocytic ehrlichiosis (Ehrlichia canis), tularemia (Francisella tularensis), Heartland virus, and a spotted-fever type of disease (Rickettsia amblyommatis is suspected to be the cause). Lone star ticks are also considered to be the main tick involved with the development of red meat allergy.
Figure 7. Lone Star Tick (Amblyomma americanum) female (L) male (R). Credit: R. Grantham Oklahoma State University
Gulf Coast Tick
[Amblyomma maculatum (Koch)]
The Gulf Coast tick (Figure 8) is a three-host tick. As larva and nymph, the Gulf Coast tick is a common pest of ground-inhabiting birds, such as meadowlarks and bobwhite quail or small rodents. The adults primarily blood feed on cattle, but a variety of other hosts including dogs, horses, sheep, deer, coyotes and humans can be parasitized. This tick has become increasingly abundant in Oklahoma in the past 20 years and is an importantpestofcattle. It transmits Hepatozoon americanum to dogs and coyotes, and possibly Rickettsia parkeri to humans. The adults attach to the ears of cattle and are most abundant in early April to mid-June. When infestations are high on cattle, the ears may become thickened and curled causing a condition called “gotch ear.” This tick reportedly has produced tick paralysis in humans and dogs.
Figure 8. Gulf Coast Tick (Amblyomma maculatum) female (L) male (R). Credit: R. Grantham Oklahoma State University
Diseases Caused by Ticks
Rocky Mountain spotted fever
Rocky Mountain spotted fever (RMSF), the most important tick-borne disease in Oklahoma, is caused by the intracellular bacteria, Rickettsia rickettsii, which is transmitted during tick feeding. Although this was first found in the Rocky Mountains, it is now mostly found in the south-Atlantic region, Pacific region, and west south-central region. Oklahoma and North Carolina have the highest incidence of the disease, accounting for more than a third of the cases annually. Most cases of RMSF in Oklahoma occur between April and September, with the peak number of cases in May, June and July. The American dog tick (Dermacentor variabilis) is the major tick that transmits RMSF, and it is most active in the spring and early summer. Most of the cases of RMSF occur in the eastern half of the state, where the American dog tick is the most abundant. Most people come in contact with this tick in heavily wooded areas, including many of the recreational areas of eastern Oklahoma.
Only a very small percentage of ticks in most areas are infected and can transmit RMSF: less than 1 in 1,000. Ticks normally transmit the disease-causing organism only when they are attached and feeding. Most scientists believe that they cannot transmit the disease until they have been attached and feeding for several hours, with some estimating at least 24 hours. However, if the tick has pre-fed on a dog, the activation time for infection could be significantly shortened. Frequent inspection and removal of all ticks at least twice a day will prevent transmission from occurring. Always record the date of tick removal and save the tick for identification for two weeks; if no illness occurs, then discard the tick. However, any change in health should be immediately reported to a medical doctor.
Symptoms of Rocky Mountain spotted fever
Usually the first symptoms of RMSF appear three days to 14 days after the tick bite. They include sudden fever, chills, muscle aches and headaches. Nervous symptoms such as sleeplessness, restlessness and delirium may also occur. In about 50 percent of patients, a characteristic spotty rash occurs on the feet and hands within two to three days of the fever. The rash may spread to the rest of the body but does not start on the trunk of the body like the rashes caused by measles and some other diseases. The development of symptoms concurrent with or after discovery of an attached tick should be followed by consultation with a medical doctor. Early diagnosis of RMSF can be effectively treated with tetracycline antibiotics, and usually results in complete recovery. If left untreated, the mortality rate can be as high as 20 percent. Two-thirds of all RMSF cases occur in children less than 15 years old, and vaccines for RMSF have not been developed.
Lyme disease
More than 30,000 cases of Lyme disease are reported annually. Lyme disease is one of the most highly publicized diseases by the news media, and because of its wide range of symptoms, has become mistakenly thought of as a common disease in Oklahoma. This disease is caused by the bacterium Borrelia burgdorferi. Despite the publicity and the great number of diagnosed cases in other parts of the U.S., Lyme disease has not been reported to have a high prevalence in Oklahoma. For the period of 1992 to 2006, within Oklahoma, the incidence of this disease averaged less than 0.7 cases per 100,000. In the northeastern U.S., the main tick carrier of the disease appears to be the nymph of the black-legged tick (Ixodes scapularis). The tick vector is abundant in Oklahoma; however, the larvae and nymphs normally feed on lizards rather than field mice, which can serve as a reservoir host for the bacteria.
Symptoms of Lyme disease
The most characteristic symptom of Lyme disease is a rash that appears in 50 to 65 percent of the cases within three days to three weeks after the tick bite. The rash, caused by erythema chronicum migrans (ECM), often expands into a ringto be associated with the site of the bite.
Lyme disease is a flu-like illness with symptoms such as fever, chills, headache, stiff neck and backache, and significant fatigue occurs with the rash. Many people have no further symptoms and recover from the infection without treatment. However, some people develop symptoms three weeks to months later,or even a year or two after the onsetof the disease. These symptoms include arthritis-like pain in the joints,tendons, muscles and bones, occurring from a week to months after the onset of the initial symptoms. Less common symptoms are numbness, tingling in the extremities, loss of concentration, sometimes a partial paralysis of the facial muscles, and in rare cases, some heart arrhythmia and palpitations. While Lyme disease rarely causes death, chronic symptoms increase with time and result in pain and long-term disability. Seeking medical evaluation and early treatment are important and can lead to resolution of Lyme disease. Untreated infections can result in permanent disability.
Southern Tick-Associated Rash Illness (STARI)
Southern tick-associated rash illness (STARI) is diagnosed by the appearance of a rash similar to the Lyme disease following lone star tick bites, and the symptoms can include fatigue, fever, headache, and muscle and joint pains. The rash of STARI is a red expanding bull’s eye lesion that develops around the tick bite. The rash usually appears within seven days of a tick bite and expands to a diameter of 3 inches or more. Unlike Lyme disease, STARI has not been linked to any arthritic, neurological or chronic symptoms. To date, the etiologic agent of STARI is unknown.
Tularemia
The cause of tularemia is the Gram-negative bacteria Francisella tularensis. Tularemia is sporadically distributed throughout most of the northern hemisphere and is a disease of many wild animals, especially rodents and rabbits, and is transmitted in nature by various species of ticks. Tularemia has been known to occur in Oklahoma since the 1920s, with most cases in eastern Oklahoma. Incidence of tularemia is sporadic with only 100 to 200 cases reported yearly from the U.S. Even though tularemia can be transmitted by handling infected animal carcasses (especially rabbits) and by ingestion of contaminated water, it is thought that most of the cases in Oklahoma are transmitted by tick bites.
Symptoms of Tularemia
The symptoms of tularemia include a flu-like illness,having an initial severe fever, temporary remission and an additional fever period of two weeks. After the initial two weeks, there are often localized lesions, possible conjunctivitis (a reddening of the mucous membranes in the eye) and enlarged, tender lymph nodes. Pulmonary complications are not uncommon and mimic community-acquired pneumonia.
Heartland Virus
Heartland virus is a recently described virus transmitted by ticks in the central U.S. As of November 2022, the CDC has recorded more than 60 cases from 14 states, including Oklahoma. To date, cases have occurred from April through September; and since first discovered, two patients have died (Dembek et al. 2024).
The virus appears to only be transmitted by lone star ticks. Because this virus was only identified in 2012, the factors that make people most at risk for acquiring Heartland virus have not yet been determined. However, like other tick-borne illnesses, those who work outside or engage in outdoor activities (hunting, hiking and walking in wooded trails) and are exposed to lone star tick bites are more likely to become infected. The onset of symptoms occurs from a few days to 2 weeks after a tick bite (Dembek et al., 2024). Similar to human monocytic ehrlichiosis, the flu-like symptoms of Heartland virus may include fever, tiredness, headache, nausea, lack of appetite, muscle aches, bruising easily and diarrhea. An identifying feature is when patients do not improve after being treated by antibiotics for seven days. Currently, there are no approved medications for the treatment or prevention of Heartland virus.
Human Monocytic Ehrlichiosis (HME)
Human monocytic ehrlichiosis (HME), transmitted by the lone star tick, is caused by the intracellular bacteria, Ehrlichia chaffeensis. The first human case was reported from Arkansas in 1986. Human cases have been found mostly in the southern states, where the lone star tick is widely distributed, and the case number has increased in recent years.
Symptoms of HME
Symptoms can range from mild to severe, and may include fever, chills, headache, aches and pains in the joints and muscles, loss of appetite, eye pain, nausea and vomiting. Development of rash is rarely reported. Hospitalization may be required.
Human Granulocytic Anaplasmosis (HGA)
Human Granulocytic Anaplasmosis (HGA) is a recently emerging tick-borne disease caused by the intracellular bacterium, Anaplasma phagocytophilum. HGA is transmitted by Ixodes scapularis ticks. White-footed mice, other small mammals and white-tailed deer can become infected and serve as reservoir hosts for A. phagocytophilum. While symptoms of this illness include fever, headache, muscle aches and tiredness, a rash is usually not apparent. HGA is increasing in all parts of the U.S. where Ixodes ticks are established.
Tick Paralysis
Tick paralysis is not a disease, but a condition caused when ticks inject saliva into the bite while feeding. Scientists are not sure whether the reaction is caused by a toxin injected with the saliva or if it is the result of a severe type of allergic reaction. This rare condition can occur in animals and humans wherever ticks are abundant. Several different tick species have been associated with tick paralysis, but in the eastern half of the U.S. including Oklahoma, it has most often been caused by the American dog tick (Dermacentor variabilis). The paralysis caused by the reaction to the toxin or other components of the saliva occurs most often when the tick is attached to the back of the head, especially near the base of the skull or near the spinal cord on the neck or back.
Symptoms of Tick Paralysis
Symptoms usually occur three days to six days after exposure to ticks and first appear as a paralysis of the hands and feet. As the tick continues to feed, paralysis moves to the face and thoracic muscles, which leads to breathing difficulty and death. Although symptoms usually appear within eight days, complete paralysis and even death has occurred within 24 hours. The most severe cases usually occur in children, often with long hair, where the feeding tick is not noticeable. Once a feeding tick is removed, the symptoms disappear in the reverse order of appearance and recovery is usually complete. When unknown paralysis occurs, one should always closely examine the patient for attached ticks.
Prevention of Tick-Borne Disease
The best way to prevent tick-borne disease is to prevent ticks from attaching and feeding for long periods. Notably, a low percentage of ticks are infected with pathogens. Ticks must be attached and feed for several days in order to transmit the pathogens that cause disease. Do not panic if you find a tick attached. Remove attached ticks by methods described in the “methods of protection from ticks” section. Be sure to record the date on a calendar and place the tick in a container in the freezer (a plastic baggie will work well for this purpose). Monitor your health for any possible symptoms of the diseases caused by ticks, and if they occur, see a medical doctor immediately. Most of the tick-borne diseases are usually easily resolved after treatment with the appropriate antibiotic, but this will depend on early diagnosis and treatment.
Methods of protection from ticks
- Avoid heavily-infested tick areas, especially in the spring and early summer.
- Stay on cleared or prepared trails or paths.
- Avoid tall grasses or bushy overgrown areas and areas covered with large amounts of leaf litter.
- Wear protective clothing.
- Wear light colored clothing, so ticks can be seen easily and removed before they attach.
- Wear long pants and tuck pant legs into boots or into high socks.
- Wrap tape (masking tape works well) around the cuffs of your pants with the sticky side out. Ticks will be captured on the tape.
- Wear boots or closed toe shoes.
- Use a repellent that indicates it works well against ticks.
- Many repellents contain DEET (N, N-diethyl-Mtoluamide) which can be placed on the skin or on clothes. Concentrations of 20% to 40% or greater work best. DEET is sold under several different trade names.
- Additional tick repellents contain the insecticide permethrin, which should be sprayed onto clothing where it remains effective for up to three washings. Do not apply to the skin. Read instructions carefully, as it is harmful to some fabrics.
- Protect your pets and premises from ticks.
- Inspect pets frequently for tick infestations. Remove ticks or treat for them.
- If your yard or premises is infested with ticks, treat it with the recommended insecticides.
- Frequently inspect yourself and other family members for the presence of ticks, especially
children, at least every two to three hours if you are in a tick-infested area.
- Examine the head and hairline especially close. The waistline and other tight spots should also be surveyed.
- Crawling, unattached ticks cannot transmit disease and are easily removed.
- Properly remove attached ticks.
- Use tweezers to grasp the tick at the surface of the skin.
- If you do not have tweezers, use tissues or a cloth to protect your fingers and to grasp the tick firmly. A ziplock bag turned inside out works very well for this purpose. (Protection of your fingers is necessary because you could accidentally crush the tick. The ticks body fluids could be infected and contaminate your fingers. You could accidentally introduce the disease organism into the mucous membranes or a scratch or wound.)
- Pull the tick straight out with a slow steady pull. Do not be alarmed if the tick head (mouthparts) stays in your skin. Your body will take care of this wound and heal without removing the head. The important thing is to stop the potential for the tick to secrete disease organisms into the feeding site by severing the connection between the tick and your skin.
- Do not try to remove ticks with a match or other hot objects, as this is likely to cause a burn. In addition, folk methods of using alcohol and Vaseline to suffocate the tick are not effective.
- Record the date of tick bite and save the tick (freeze in the ziplock bag used for removal) in case you become ill.
- To prevent tick populations from building up in your yard, keep ticks off your pets,
keep your lawn mowed and prevent the growth of tall grass, weeds or brush in fence
lines and around shrubbery.
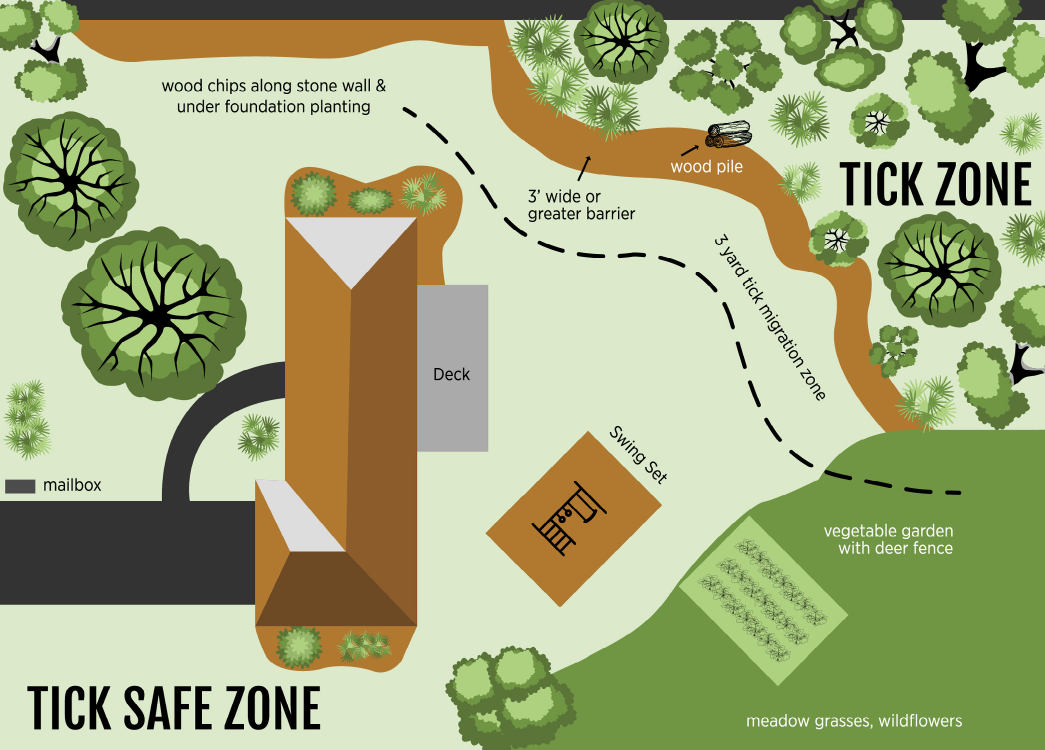
- Landscaping Tips to Reduce or Limit Tick Access to Your Property:
- Remove leaf litter and clear tall grasses and brush around homes and at the edges of lawns.
- Place wood chips or gravel between lawns and wooded areas to restrict tick migration to recreational areas.
- Mow the lawn and clear brush and leaf litter frequently.
- Keep the ground under bird feeders clean.
- Stack wood neatly and in dry areas.
- Keep playground equipment, decks and patios away from yard edges and trees.
- Do not use pet tick and flea collars on humans to repel ticks.
- Discourage deer from entering your lawn.
- Bait boxes that treat wild rodents with acaricide (insecticide that kills ticks) are now available for home use. Properly used, these boxes have been shown to reduce ticks around homes by more than 50%. The treatment is similar to products used to control fleas and ticks on pets; it does not harm the rodents. Bait boxes are available from licensed pest control companies.
Figure 9. Landscaping for homeowners to provide a tick migration zone for targeted pesticide applications. www.cdc.gov
References
Dembek, Z.F. J.L. Mothershead, C.M. Cirimotich, and A. Wu. 2024.Heartland Virus Disease - An Underreported Emerging Infection. Microorganisms 12(2), 286.www.mdpi.com