Electronic Medical Records: What are They
During the past few years, there has been an increasing amount of discussion in the health care industry regarding the use of Electronic Medical Records (EMRs). In general, an EMR is a medical record in digital format that provides all relevant information about a patient in one single location. A more formal definition is, “a system that integrates electronically-originated and maintained patient-level clinical information, derived from multiple sources, into one point of access” (American Hospital Association, 2007). EMRs are usually included in conversations regarding improving quality of care, lowering costs, and increasing overall efficiency. EMRs have been implemented by hospitals, physician offices, and other ambulatory environments. A true EMR includes all relevant patient information such as:
- Vital signs
- Orders from physicians
- Physician’s notes
- Laboratory results
- Prescriptions
- Progress notes
- Nursing documentation
- Radiology orders
Although some systems employ only a subset of these modules, the long-term focus of EMRs is to provide a fully-functional technology that can capture all relevant information for the facility in which it is placed.
The Obama administration has called for providing electronic patient records throughout the country before the year 2014, and the 2009 economic stimulus bill contains significant funding (nearly $20 billion) to promote this effort. This includes sizeable incentives, both for individual physicians who document they are meaningfully using the technology (between $40,000 and $60,000 over 5 years) and for hospitals (who can be eligible for several million dollars in Medicare and Medicaid reimbursements) (King, 2009).
This document attempts to explain what electronic medical records are, who can benefit from using them, and the process that a hospital typically undertakes to implement this technology. A discussion of the barriers and limitations associated with EMRs will also be provided, along with information on programs available in Oklahoma to help rural hospitals and physicians through EMR selection and implementation.
Who is Using Them?
Both physicians and hospitals have slowly begun to increase their use of EMRs. Although statistics on exactly how many physicians or hospitals are taking advantage of EMRs are vague, surveys suggest that around 20 to 25 percent of physicians were using an EMR system in 2006 (Robert Wood Johnson Foundation, 2006; Jha et al., 2006) while estimates of hospital EMR usage ranged from 20 to 30 percent (Fonkych and Taylor, 2005). However, only 10 percent of physicians are using a fully functional EMR system that incorporates all aspects of a patient visit, from collecting patient information to entering medical orders and prescriptions. A more recent survey on physician usage by the Center for Disease Control found that 20 percent of physicians were using “minimally-functioning” EMR systems, which includes the capability to place orders for prescriptions and tests, the ability to view laboratory or imaging results, and the ability to capture clinical notes (Hsiao et al., 2008). Other surveys have found that hospital use of EMRs varies dramatically by ownership type, with only 5 percent of public hospitals using EMRs, compared with 14 percent of for-profit hospitals and 73 percent of non-profit hospitals (Kazley and Oscan, 2007). Table 1 compares EMR adoption rates for physician offices of multiple sizes and for hospitals as well.
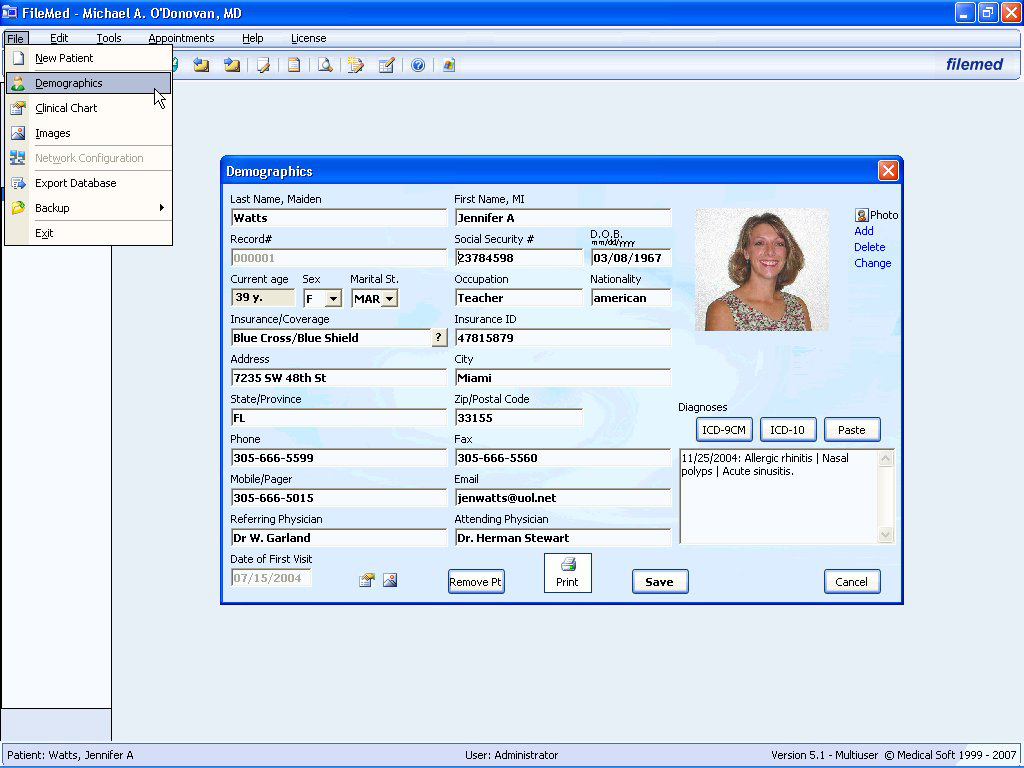
Photo: www.filetransit.com/screenshot.php?id=33989
| Table 1. EMR Adoption Rates among Physicians and Hospitals. | |
| Type of Facility | Percentage of Adoption |
| EMRs in physician offices | 17 to 25% |
| Solo practitioners | 13 to 16% |
| Large physician offices (>20) | 19 to 57% |
| EMRs in hospitals | 20 to 30% |
| Source: Robert Wood Johnson Foundation, 2006; Fonkych and Taylor, 2005. |
What are the Benefits?
Proponents of EMR systems have claimed they offer a wide variety of benefits. The most common benefits are:
- Improved safety
- Improved quality of care
- Long-term cost savings
- Greater efficiency
Some of these benefits are theoretical, while others have been documented from actual use. Many of the proposed benefits were apparent even in the 1990s – one 520-bed hospital in Utah decreased mortality rates by 1 percent, reduced antibiotic use by 22 percent, increased appropriate post-surgery antibiotic use from 40 to 99 percent, and dropped adverse drug events by 30 percent after EMR implementation in 1996 (Hannan, 1999). One appealing benefit that is still under debate is the cost associated with the system. While long-term cost savings are expected, most EMR systems are still new enough to prevent accurate pre/post cost comparisons. Some cost savings are expected immediately (such as reduced man-hours for paper filing/retrieval), while cost savings from improved workflow could take several months or even years to accrue. At an aggregate level, Hillestad et al. (2005) hypothesized that with a 90 percent EMR adoption rate, the nation could average more than $77 billion in savings per year due to the higher efficiency associated with EMRs. This $77 billion includes savings from avoiding adverse drug effects, improved workforce productivity, and potential reductions in malpractice premiums due to the presence of automated reminders for drug-to-drug and drug-to-allergy interactions.
The types of improvements noted above can also improve the quality of care offered at a hospital or medical office. If critical lab values fall outside of a normal range, they can immediately be flagged for further inspection. Further, priorities can quickly be set for each patient, and automated notes to apply specific medications can serve as timely reminders. Decreased diagnosis time, quicker workflow, and automated discharge instructions are other ways in which the EMR will improve the overall quality of care and create a more efficient environment.
Recent EMR adoptees have also lauded the ability of their system to correctly capture all potential charges due to built-in charge codes associated with specific diagnoses, eliminating the problems of “up-coding” (charging more than is necessary) and “down-coding” (charging less than is necessary). This feature also provides its users with the peace of mind associated with knowing they are fully documented if an audit of their charges should occur.
What are the Barriers?
While there are numerous benefits, there are still limitations and barriers to implementing an EMR system. The most common barriers that are:
- Up-front costs
- Training time (personnel already have full-time jobs)
- Uncertainty about information security
- Physician/employee resistance or attitudes
The cost to install an EMR system is typically a large roadblock, particularly for smaller hospitals or physician offices. The upfront cost can be substantially large. Miller and Sim (2004) found that up-front costs for a physician office EMR system can range from $16,000 to $36,000 per physician. For rural hospitals, implementation costs can vary significantly depending on the system chosen and capability included. Four rural hospitals in Oklahoma that began implementation of their EMRs during 2008 – 2009 experienced up-front costs ranging from $300,000 to $1,700,000.
Along with the high cost of the hardware and software, there are also costs associated with training physicians and staff. While the vendor usually provides initial training once the system is ready for use, it may be several months before physicians and staff feel comfortable using it. Additionally, the staff at most rural hospitals are typically quite busy and scheduling large blocks of time for them to attend training sessions can be challenging. For many, the technology is new and is significantly different from usual patient to patient routines.
Miller and Sim (2004) found that this “learning period” can be considerable – most physicians increased the time they spent per patient after the implementation of EMRs for a period ranging from a few months to several years. This can be costly in terms of lost revenue and in the general attitude toward the technology. In fact, one of the key findings of a 2007 survey of more than 285 practices with recent EMR adoption was that increased operating costs and reduced productivity should be expected during the first 6 to 24 months of implementation (MGMA, 2007). However, the survey also notes that after this initial period, the benefits of EMR adoption should increasingly outweigh the costs.
One common concern with EMRs is the question of information security. Who will have access to the records, and how do patients know their personal records will not be shared? Thankfully, almost all EMR systems on the market today are compliant with the Health Insurance Portability and Accountability Act (HIPAA), which addresses the security and privacy of health data. Since each employee has a unique log-on, the systems automatically collect data on the screens viewed or printed by a particular employee, allowing for traceability and flagging questionable activity. So, although some patients may have concerns about their information being made available electronically, the systems on the market have already taken steps to minimize any security problems.
Another important barrier is employee attitudes toward EMRs. Due to misconceptions and horror stories, many administrators, physicians, and even the general public have formed a fear of EMRs. These misconceptions include that EMRs will not improve the quality of care, that they are just one big mess, that they will take too long to learn, or that they will just get in the way. There are many who believe there is nothing wrong with their current system and see no reason to switch to EMRs.

Photo: Drumright Regional Hospital
While these barriers may be based on realistic concerns, there is significant evidence to suggest that EMRs are here to stay. Convincing employees (particularly the physicians) that moving to an EMR system is the correct move for their organization is critical to getting the buy-in necessary for the system to work. This can be accomplished through case studies (such as those documented in this fact sheet or in other research listed below) or by recognizing current inefficiencies in your own workflow where EMRs can contribute. Table 2 below summarizes the overall benefits and barriers that occur when moving to an EMR system.
Table 2: EMR Benefits and Barriers.
|
Benefits |
Barriers |
|---|---|
|
Lowered operating costs |
Start-up costs |
|
Improved safety |
Training time involved at start-up |
|
Improved quality of care |
Information security concerns |
|
Efficiency: Coding help/documentation in case of an audit |
Employee resistance |
Types of EMR Systems
There are two primary types of EMR systems that hospitals or physicians typically use:
- ASP, or Web-based – this is a remotely-hosted software system accessed via an Internet web browser, similar to the model used in online banking.
- Client /server – the server for this system physically resides at the hospital or physician office, and the EMR software is run from the desktop of the computers on-site.
The primary difference between the two is that the ASP model has a remotely-located server, which means the company with whom you contract is responsible for HIPAA compliance and technical management. The up-front cost of a client / server system is therefore higher (since you are paying for the hardware), but the maintenance costs are lower than they would be with an ASP system. Maintenance costs can vary significantly, but typically range from $2,000 to $8,000 per month for a hospital. Some of the pros and cons associated with these two types of systems are shown in Table 3.

Photo: Drumright Regional Hospital
Table 3: Pros and Cons of ASP and Client / Server EMRs.
| PRO | CON | |
|---|---|---|
| ASP / Web-based | Low initial cost | Not in possession of own data |
| System maintained by IT professionals | Dependent on Internet connection | |
| Available from anywhere with an Internet connection | Contracts longer/harder to end | |
| Client / Server | In possession of own data | Higher initial cost |
| Not dependent on Internet connection | Manual updates usually required | |
| Better integration with imaging devices and on-site resources | Remote access to EMR is limited |
How to get started
The most important step for physicians or hospitals considering EMR implementation is to consult with someone with considerable experience on the topic or someone who has gone through the process already. In the state of Oklahoma, the OSU Center for Health Sciences is specifically focused on providing assistance to rural physicians and hospitals. Chief medical information officer Jason Bray has not only helped many rural hospitals select and implement their EMR systems, but is also working on selecting an EMR for the entire OSU clinical system. Future plans for the Center include offering web-based EMR systems to individual doctors for a specified monthly cost. Mr. Bray has a significant amount of experience with health information technology both in and outside Oklahoma, and his many contacts in the industry have made the EMR implementation process much easier for numerous hospitals across the state.
The selection of a vendor usually takes around 16 weeks, broken out in the following pieces:
- Request for Information: 4 weeks
- Request for Proposals: 4 weeks
- Vendor Demonstrations: 8 weeks
The first step of this process (which Mr. Bray and OSU can help walk a facility through) is to identify overall expectations of the system and define what a hospital or physician could get out of the new technology. From there, it can be determined what technology exists that would meet the demands, needs, and overall expectations of a particular facility. This consists of writing an RFI (Request for Information) which tells vendors about the general facility environment, the information technology and network environment, and the desired date of implementation. After roughly four weeks of gathering and reviewing the responses, formal RFPs (Request for Proposals) are sent out asking for detailed information from vendors to propose a system to be used at your facility. Allowing another four weeks to receive and review the RFPs, the systems are then narrowed down to the top few (usually two or three). These systems will then be set up for on-site demonstrations, so decision-makers can see the system in use and determine which system is preferred overall. These demonstrations usually take place in other hospitals or offices where the EMR is already operating, so the individuals involved in the selection process can compare it to their own situation and ask appropriate questions. This part of the process takes an average of 8 weeks to complete. It is imperative that physicians and administrators agree on the system to be selected to avoid problems further down the line.
Once the vendor has been selected, several additional weeks (or, more often, months) will be required to implement the hardware and software on-site and to permit training of hospital or office personnel. Switching from traditional recordkeeping to electronic records affects everyone from administrators to aides, so they should at least understand why it is being done and how it will impact their job.
The total time frame, from the beginning of the vendor selection to full implementation of a system, generally ranges between 12 and 18 months.
The worst possible outcome for an office or a hospital is to get halfway through a selection process only to determine that the systems being looked at simply will not work for the facility in question. In some cases, hospitals have gone through the entire selection process and begun implementation of the system only to discover that they chose the wrong one. Re-starting the process lost these facilities more than two years and hundreds of thousands of dollars, which is why working with someone who has real-world experience and an objective view of the entire process is so crucial. Writing out and reviewing RFIs and RFPs is not something usually handled by hospital personnel, so working alongside someone who knows what questions to ask and what to look for in the response is imperative.
Summary
With the mandates of 2014 edging closer, more hospitals and physicians offices will be looking towards EMR systems in the near future. While the benefits of long-term cost savings, quality of care, safety improvements, and efficiency make a solid case for EMR implementation, there are still common barriers of the up-front cost, the time required for training, and resistance from employees. When a facility does decide to move towards electronic records, there are several factors and steps to consider. One of the most important steps to getting started is to contact and consult with someone who has gone through the process already. For those within the state of Oklahoma, Jason Bray at the OSU Center for Health Sciences is an excellent person to contact to help make the process as smooth as possible. Regardless of the system selected or the amount of time it takes to choose a system, it is imperative that the system “fits” and the employees support the change. EMRs can prove to be very beneficial to a hospital or physician office when everyone understands their value and is willing to contribute to the implementation process.
Possible Vendors
- Epic: https://www.epic.com
- Praxis: https://www.praxisemr.com/
- EMR Experts: http://www.emrexperts.com
- Meditech: http://www.meditech.com
- E-Clinical Works: http://eclinicalworks.com
- Cerner: https://www.cerner.com/
Contact:
Brian Whitacre, Ph.D.
Assistant Professor and Extension Economist
Oklahoma Cooperative Extension Service
504 Ag Hall
Oklahoma State University, Stillwater, OK
Jason Bray, MBA, MHA
Chief Medical Information Officer
OSU Center for Health Sciences
2345 SW Blvd
Tulsa, OK
References
Burt, C. and E. Hing. 2005. “Use of Computerized Clinical Support Systems in Medical Seettings: U.S., 2001-03.” Advance Data. 353:1-8.
Fonkych, K. and R. Taylor. 2005. “The State and Pattern of Health Information Technology.” RAND Corporation: California.
Hannan, T. “Variation in Health Care – The Roles of the Electronic Medical Record.” 1999. International Journal of Medical Informatics. 54(2): 127-136.
Hillestad, R., J. Bigelow, A. Bower, F. Girosi, R. Meili, R. Scoville, and R. Taylor. 2005. “Can Electronic Medical Record Systems Transform Health Care? Potential Health Benefits, Savings, and Costs.” Health Affairs. 24(5):1103-1117.
Jha, A., T. Ferris, K. Donelan, C. DesRoches, A. Shields, S. Rosenbaum, D. Blumenthal. 2006. “How common are electronic health records in the United States? A Summary of the Evidence.” Health Affairs Web Exclusive.
Kazley, A. and Y. Ozcan. 2007. “Organizational and Environmental Determinants of Hospital EMR Adoption: A National Study.” Journal of Medical Systems. 31: 375-384.
King, P. 2009. “Stimulus Package and EMR Use by Physicians.” Available at www.netdoc.com.
Medical Group Management Association. 2009. “Electronic Health Records: Perspectives from the Adopters.”
Miller, R. and I. Sim. 2004. “Physicians’ Use of Electronic Medical Records: Barriers and Solutions.” Health Affairs. 23(2):116-126.
Robert Wood Johnson Foundation. 2006. “Health Information Technology Foundation in the United States: The Information Base for Progress.” Available at www.rwjf.org/files/publications/other/EHRReport0609.pdf
Brian Whitacre, PhD
Assistant Professor and Extension Economist
Lara Brooks, MS
Assistant Extension State Specialist
Jason Bray, MBA, MHA
Chief Medical Information Officer,
OSU College of Osteopathic Medicine
